“Complexity, invasiveness and length of Cardiac Surgeries stimulate the inflammatory response activation and the development of a postoperative SIRS“
Each year approximately 1.5 million open-heart interventions are performed, with 500,000 procedures in Europe, as many in the United States and in Italy are about 60000 per year.

Although there have been significant advances in perfusion technologies and biocompatible materials used in CPB, patients undergoing complex cardiac surgery procedures such as re-operative coronary artery bypass grafting (redo-CABG), multiple interventions, aortic reconstruction, valve replacement due to endocarditis, or hypothermic circulatory arrest, remain at significantly higher risk of having complications, ranging from short-term organ dysfunction to multiple organ failure and death.
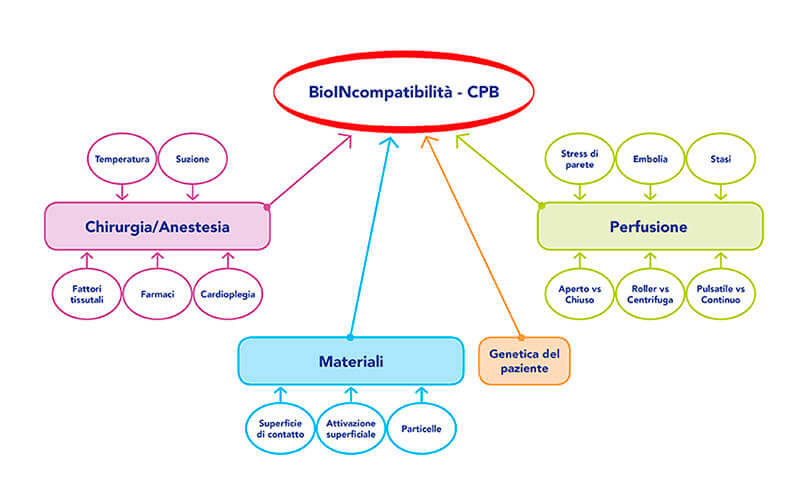
Factors such as the trauma of the surgical procedure, non-pulsatile blood flow, ischemia-reperfusion injury, and blood contact with air and artificial surfaces of the CPB system can lead to an activation of the complement system and a stimulus of inflammatory cytokine production. The concentration of these inflammatory mediators is directly correlated to the complexity, length, and invasiveness of the surgery and can lead to a post-operative systemic inflammatory response syndrome (SIRS) with SIRS-related complications such as acute kidney injury, respiratory and circulatory failure.
Furthermore, shear forces and cardiotomy suction can cause hemolysis resulting in the release of free hemoglobin, an important contributor to post-operative kidney injury. The acute kidney injury (AKI) occurs in up to 30% of patients undergoing on-pump cardiac surgery and is associated with mortality rates ranging from 7% to 38%. The 5% of these patients will develop renal failure requiring hemodialysis with a substantially higher risk of death ranging from 50% to 90%.
The cannulation of the fermoral artery during ECMO, complications that may occur during CEC and ischemia of the limbs with subsequent reperfusion may lead to muscle degradation with release of myoglobin into the circulation. The myoglobin, accumulating at the renal tubular level, is able to damage its function and bring the patient into irreversible renal failure.
To date, there are extracorporeal treatments of adsorption of cytokines and other degradation products of hepatic and renal function such as bilirubin, free haemoglobin and myoglobin, potentially able to reduce post-operative complications and costs.
The use of these devices can be developed in three directions:
The integration of these methods on all extracorporeal circuits (CPB, ECMO, CRRT) makes possible the application of the methods in various areas, including:
- Long CPB duration expected (>120 min)
- Combination procedures (valve repair/replacement, with endocarditis, CABG)
- Redo procedures
- Heart transplantation
- Aortic surgery
- Hyperbilirubinemia/rhabdomyolysis
- Circulatory arrest (>20 min)
- Patients with multiple comorbidities and/or pre-existing hepatic and/or renal dysfunction
- High risk of developing intra- and post-operative complications related to hyperinflammation
